 When the Kidneys Stop Working
When the Kidneys Stop Working
Kidneys play a crucial role in keeping the body balanced. These small, bean-shaped organs filter waste, control fluid levels, and regulate blood pressure. When kidneys lose about 85-90% of their function, the condition is known as end-stage renal disease (ESRD). At this point, kidneys can no longer support the body’s needs, making medical intervention essential for survival.
The buildup of waste in the blood leads to a range of complications—fatigue, nausea, difficulty breathing, and confusion are just the start. Without functioning kidneys, excess potassium can cause irregular heartbeats. Likewise, the body struggles to produce erythropoietin, which leads to anemia and weakness. This late-stage kidney failure demands either dialysis or a kidney transplant to keep the patient alive.
One key factor leading to ESRD is high blood pressure. Constantly elevated pressure damages the tiny blood vessels in the kidneys. Over time, they can no longer perform their filtration duties. Diabetes is another major culprit—high blood sugar damages the filtering units called nephrons. When both diabetes and hypertension are present, the risk of kidney failure multiplies.
Early Signs and Symptoms of Kidney Failure
How to Know If Something’s Wrong
Recognizing the early signs of kidney failure is critical. Symptoms often sneak up slowly, which is why they’re easy to ignore. Early on, a person may feel more tired than usual or notice swelling in their ankles or face due to fluid retention. These mild symptoms gradually grow worse as kidney function drops.
By the time end-stage renal disease develops, the signs become severe and hard to ignore. Patients may feel nauseous often, lose their appetite, experience muscle cramps, and have difficulty concentrating. Itching due to the buildup of toxins under the skin is common. Urine output also decreases or becomes foamy due to protein loss.
Another red flag is high blood pressure that doesn’t respond well to medications. The kidneys help regulate blood pressure, so failure affects this balance. Some people may also experience sleep disturbances or restless leg syndrome—problems often linked to waste buildup in the bloodstream.
Routine lab tests can help catch declining kidney function. Blood tests for creatinine and BUN (blood urea nitrogen) reveal how well kidneys are filtering. Urine tests showing protein or blood may also point to underlying kidney damage. Early detection is key to slowing the progression toward ESRD.
Causes Behind Kidney Failure
What Leads to Total Kidney Shutdown
Multiple factors can contribute to the development of kidney failure. Diabetes is by far the most common. Over time, high blood sugar damages the small filtering units inside the kidneys. This is referred to as diabetic kidney disease, a condition that affects millions of individuals and is a primary reason for the rise in kidney failure cases.
Hypertension is another major cause. High blood pressure strains the blood vessels, including those in the kidneys, which leads to scarring and permanent damage. Other causes include glomerulonephritis (an inflammation of the filtering parts), polycystic kidney disease (a genetic disorder), and prolonged urinary tract obstructions due to kidney stones or an enlarged prostate.
Autoimmune conditions like lupus can also damage the kidneys, as can infections and certain medications, especially overuse of painkillers like NSAIDs. Exposure to toxins in the environment or workplace may also play a role. Regardless of the cause, all lead to the same outcome—gradual loss of kidney function until reaching end-stage renal disease.
Sometimes, kidney failure happens suddenly. This is called acute kidney injury (AKI), usually triggered by severe infections, dehydration, or sudden trauma. While AKI can often be reversed if treated quickly, if left untreated, it may lead to chronic kidney disease and ultimately ESRD.
Treatment Options for ESRD
Choosing Between Dialysis and Transplant
When kidneys can no longer do their job, the patient faces a life-changing decision: dialysis or kidney transplant. Dialysis is a treatment that filters and purifies the blood using a machine. There are two types—hemodialysis and peritoneal dialysis. Hemodialysis is typically done at a clinic three times a week. Peritoneal dialysis, on the other hand, can be performed at home, offering more flexibility.
A kidney transplant involves replacing the damaged kidneys with a healthy one from a donor. This option offers the best long-term results and improved quality of life, but it comes with challenges—availability of a donor, risk of rejection, and the lifelong need for immunosuppressant medications.
Patients must also follow strict lifestyle changes, regardless of the treatment method. A kidney-friendly diet, low in sodium, potassium, and phosphorus, becomes essential. Fluid intake must be carefully controlled. Medications to manage blood pressure, anemia, and bone health are also necessary.
The goal of all treatments is to manage symptoms, prevent complications, and enhance life expectancy. Education and counseling are important to help patients make informed choices. Proper support from healthcare providers, family, and patient groups plays a vital role in managing life with end-stage renal disease.
Living With ESRD: What to Expect Daily
Adjusting to a New Lifestyle
Living with end-stage renal disease is challenging but manageable with the right approach. Daily routines revolve around treatment schedules, medication, diet restrictions, and regular checkups. Emotional health can be deeply affected, leading many to experience anxiety or depression. That’s why mental health support is just as vital as physical treatment.
Patients on dialysis may experience fatigue after sessions, dietary limits, and fluid restrictions. However, many continue to work, pursue hobbies, and enjoy life. It’s all about planning and balancing activities with health requirements.
Staying informed is one of the best tools for managing this condition. Understanding the cause of ESRD, knowing how to monitor symptoms, and actively participating in treatment decisions empower patients. Peer support groups, online communities, and kidney disease education programs can offer both information and emotional backing.
Proper management of other health conditions like diabetes or high blood pressure is essential to prevent further complications. Regular monitoring and adapting to changes in health help maintain stability. Many ESRD patients lead fulfilling lives by making health a priority and leaning on their support systems.
.
Nutrition and Diet for Kidney Failure
What to Eat and What to Avoid
Diet becomes a key factor in managing end-stage renal disease. Since the kidneys can no longer filter waste properly, eating the right foods helps reduce the workload on them. A renal diet focuses on controlling levels of sodium, potassium, phosphorus, and protein to prevent buildup of harmful substances in the blood.
Patients are often advised to reduce salt intake significantly. Too much sodium can cause high blood pressure and fluid retention, leading to swelling and heart problems. Avoiding canned foods, processed meats, and salty snacks can help keep sodium levels in check.
Potassium, though important for muscles and nerves, must also be monitored. When kidneys fail, potassium levels can rise to dangerous levels, affecting heart rhythm. Bananas, oranges, tomatoes, and potatoes are high in potassium and are typically limited. Instead, apples, grapes, berries, and cauliflower are preferred.
Phosphorus is another mineral to watch. Excess phosphorus can lead to bone issues and itchy skin. Dairy products, cola drinks, and nuts are high in phosphorus and should be consumed sparingly. Phosphate binders are often prescribed to help control levels in the body.
Protein intake is a bit of a balancing act. While the body needs protein to maintain muscle and repair tissues, too much can lead to more waste buildup. Patients are usually guided to consume moderate amounts of high-quality proteins like eggs, fish, and lean meats under the supervision of a renal dietitian.
Fluids are often restricted as well. With failing kidneys, fluid buildup can lead to swelling, shortness of breath, and high blood pressure. The daily fluid limit depends on how much urine the patient produces and whether they’re on dialysis.
Meal planning, label reading, and consulting a kidney dietitian can make a huge difference. Adjusting the diet not only eases symptoms but also enhances quality of life for those with end-stage renal disease.
Preventing Further Kidney Damage
How to Slow Down the Progression
For those who haven’t yet reached ESRD but are dealing with chronic kidney disease (CKD), slowing down progression is crucial. Proper management can delay or even prevent the onset of end-stage renal disease. It all starts with managing underlying conditions like diabetes and high blood pressure.
Maintaining healthy blood sugar levels is essential for diabetics. Monitoring glucose regularly, sticking to a diabetes-friendly diet, and taking medications as prescribed can protect the kidneys. Similarly, controlling blood pressure with lifestyle changes and medications helps reduce kidney strain.
Avoiding over-the-counter pain medications like NSAIDs (ibuprofen, naproxen) can also protect kidney health. These drugs, when used frequently, can damage the filtering units and accelerate kidney decline. It’s best to use them sparingly and under medical supervision.
Staying hydrated helps, but fluid intake should be balanced—especially for those at risk of fluid overload. Smoking cessation, regular exercise, and maintaining a healthy weight are lifestyle habits that support kidney function.
Monitoring kidney function through routine lab tests is vital. Tracking creatinine, BUN, eGFR (estimated glomerular filtration rate), and urine albumin levels offers early signs of worsening kidney health. Early intervention is the best strategy for preventing end-stage renal disease.
Emotional Impact of Kidney Failure
Mental Health and Coping Strategies
The psychological effects of kidney failure are often underestimated. A diagnosis of end-stage renal disease is life-changing, bringing emotional stress, fear of the unknown, and lifestyle disruptions. Patients commonly experience anxiety, depression, and feelings of isolation.
Accepting the condition is the first emotional hurdle. It takes time to come to terms with the reality of chronic dialysis or the waiting game for a transplant. Support from mental health professionals, family, and support groups is essential during this time.
Counseling, whether one-on-one or group therapy, offers a space to express fears, frustrations, and grief. Cognitive Behavioral Therapy (CBT) has proven effective for many ESRD patients. It helps reframe negative thoughts and develop healthy coping mechanisms.
Connecting with others going through similar experiences can also offer comfort. Peer support groups or online forums allow patients to share tips, vent emotions, and feel less alone. Encouragement and shared wisdom can uplift mental spirits during tough days.
It’s also important for caregivers to monitor their own mental health. The emotional toll of supporting a loved one through kidney failure is heavy. Seeking guidance, sharing responsibilities, and scheduling self-care breaks can reduce burnout.
Daily routines that include stress-relieving activities like walking, meditation, journaling, or hobbies can make a huge difference. Managing emotional well-being is just as vital as physical treatment for those living with end-stage renal disease.
Children and ESRD: A Different Battle
Unique Challenges Faced by Pediatric Patients
While kidney failure in adults is well-known, children can also develop end-stage renal disease. The causes are often different—congenital abnormalities, genetic conditions, or autoimmune disorders like nephrotic syndrome top the list. Unlike adults, pediatric patients may not show symptoms early, making diagnosis tricky until kidney function is already compromised.
The treatment options for children are similar—dialysis or kidney transplant. However, dialysis can be especially tough on a child’s small body. Growth delays, learning difficulties, and emotional distress often accompany treatment. Transplants offer better long-term outcomes for kids, but finding a suitable donor is often more challenging due to size and compatibility issues.
Pediatric nephrologists work closely with families to manage not just the physical but also the emotional and social effects. Kids may struggle to understand why they can’t eat certain foods, go to school every day, or play sports like their peers. Regular counseling and educational support become critical components of their care.
Parents play a key role in monitoring symptoms, managing medications, and ensuring adherence to treatment plans. They often need to adjust work schedules, finances, and lifestyles to accommodate their child’s needs. Fortunately, advances in pediatric kidney care have improved survival and quality of life for many young ESRD patients.
Technological Advancements in Kidney Care
How Innovation Is Changing Lives
The management of end-stage renal disease is undergoing a quiet revolution thanks to technology. From better dialysis machines to wearable kidney devices, innovation is enhancing patient comfort and treatment efficiency.
Modern hemodialysis machines now offer more accurate filtration and customized settings for individual patient needs. They’re more portable and quieter, making in-home dialysis more practical. Meanwhile, peritoneal dialysis machines are becoming smarter, offering night-time therapy without disturbing sleep patterns.
Wearable artificial kidneys are currently in clinical trials. These compact devices promise continuous dialysis on the go, reducing the need for clinic visits and offering greater lifestyle flexibility. Though not widely available yet, they signal a hopeful future.
Telemedicine has also made it easier for ESRD patients to connect with nephrologists without long travel. Virtual consultations help manage symptoms, review test results, and adjust medications with ease—especially for rural or immobile patients.
Additionally, machine learning is helping identify patients at risk of kidney failure earlier than ever. AI-driven tools analyze lab results and medical histories to predict who might benefit from preventive care. These insights allow doctors to intervene before ESRD sets in.
Innovation isn’t just about machines. New medications to manage anemia, control phosphorus levels, and protect the heart are continually being developed. As research progresses, the future for ESRD patients looks increasingly hopeful.
Conclusion
Understanding end-stage renal disease is vital—not just for patients, but for anyone who wants to protect their health. Kidney failure isn’t an overnight event. It often develops silently over time due to unmanaged conditions like diabetes or high blood pressure. Recognizing early symptoms, staying on top of regular health screenings, and making healthy lifestyle choices are crucial steps in prevention.
For those living with ESRD, treatment choices like dialysis and transplants, alongside proper diet and emotional care, allow many to continue living active, meaningful lives. New technology and ongoing research are opening doors to better care and improved quality of life.
Whether it’s managing the challenges of diet, adapting to daily dialysis, or coping with the emotional toll, support and knowledge go a long way. With medical advancements and strong care networks, ESRD doesn’t have to mean the end—it can be the beginning of a new way of life.
FAQs
- What causes kidneys to fail in the first place?
The most common causes are diabetes and high blood pressure. Other reasons include genetic disorders, autoimmune diseases, and infections. - How long can someone live with ESRD on dialysis?
With proper treatment, many people live for years on dialysis. Life expectancy depends on age, overall health, and how well other conditions are managed. - Is a kidney transplant always better than dialysis?
Generally, yes. A transplant often improves quality of life and survival, but not everyone is a suitable candidate due to other health factors. - Can ESRD be cured?
No, ESRD cannot be reversed. However, kidney transplants can restore kidney function, and dialysis can manage symptoms effectively.
5. Are there any new treatments coming soon for ESRD?
Yes, wearable artificial kidneys, advanced dialysis machines, and AI-based predictive tools are currently in development and show promising results.
- When Your Kidneys Fail: Understanding ESRD
- Discover what happens when kidneys fail, including causes, symptoms, and treatment options for End-Stage Renal Disease (ESRD).
- Health, Kidney Disease, ESRD, end-stage renal disease, dialysis, kidney failure, nephrology
Related posts:
 Best Topical Finasteride & Minoxidil Spray for Hair Regrowth
Best Topical Finasteride & Minoxidil Spray for Hair Regrowth
 What Are the Key Considerations Before Getting Filler Injections?
What Are the Key Considerations Before Getting Filler Injections?
 Dr. Kami Hoss Gives Out the Truth About Brushing & Flossing-Protecting Your Teeth
Dr. Kami Hoss Gives Out the Truth About Brushing & Flossing-Protecting Your Teeth
 Can Atrial Fibrillation Be Cured? Latest Research & Insights
Can Atrial Fibrillation Be Cured? Latest Research & Insights
 Prozenith: A Natural Weight Loss Supplement 70% OFF Discount
Prozenith: A Natural Weight Loss Supplement 70% OFF Discount
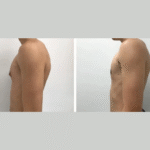 Recovery and Aftercare Tips for Gynecomastia Patients in Dubai
Recovery and Aftercare Tips for Gynecomastia Patients in Dubai
 Top Reasons to Choose a Vitamin D3 Soft Gel for Everyday Health
Top Reasons to Choose a Vitamin D3 Soft Gel for Everyday Health
 Common Dental Emergencies and How Dentists Handle Them: Complete Guide
Common Dental Emergencies and How Dentists Handle Them: Complete Guide







